Health Policy & Advocacy


Health policy work conducted in the Division of General Internal Medicine is unified by a firm commitment to improve conditions and policies to enhance the health and well-being of vulnerable populations. Listed below are descriptions of some of our faculty members' current policy work.
Soraya Azari, MD
Dr. Azari’s health policy interest relates to the use of opioid medications for treatment of chronic, non-cancer pain. She is part of a working group comprised of San Francisco safety net providers who aim to devise best practices for use of opioids in primary care. Her group has drafted quality standards for participant clinics, and is collaborating with local emergency departments to discuss appropriate use of opioids.
Kirsten Bibbins-Domingo, MD
Dr. Bibbins-Domingo current work focuses on understanding the interaction between social, behavioral, and biological factors that place vulnerable groups at risk for cardiovascular disease early in life and population-wide policy level interventions that may prevent disease in these groups. She has provided recommendations to local, state, federal, and international organizations interested in the impact on food and nutrition policies on cardiovascular disease prevention and health disparities, including the California Department of Public Health, the Centers for Disease Control and Prevention (CDC), and the Pan American Health Organization (PAHO). She has served on several committees of the Institute of Medicine (IOM), advising federal agencies on policies related to adverse effects of vaccines, presumptive disability in veterans, valuing community-based prevention, and evaluating the impact of population-wide sodium reduction. She is a member of the US Preventive Services Task Force that develops national guidelines for clinical prevention.
Maria Chao, MD
Dr. Chao’s policy and advocacy efforts focus on improving access to evidence-based complementary and integrative medicine for underserved populations. Her current work includes broadening non-pharmacologic options for pain management in primary care and evaluating the implementation of acupuncture in safety net settings to improve quality of life among patients with chronic conditions. She has published on racial/ethnic differences in reasons for using complementary health approaches, factors that affect disclosure of complementary medicine use to healthcare providers, and socioeconomic access to integrative health through group-based models. Dr. Chao is a member of the steering committee for the Integrative Pain Management Program of the San Francisco Health Network. She co-chairs a Working group on Traditional and Complementary Medicine Research in Asian American Communities and serves on the Board of Directors Integrative Medicine for the Underserved, a national multi-disciplinary organization committed to affordable, accessible integrative health care for all.
Alicia Fernandez, MD
Dr. Fernandez’s policy work has primarily focused on issues affecting US minority and immigrant populations related to chronic disease care. She is particularly interested in language barriers in health care and the associated policy implications regarding physician language ability and professional interpreter use. Her work in this area has included research on: the impact of language barriers on the management of Type 2 diabetes among Latinos; resident physicians’ use of professional interpreters; the accuracy of tools used to assess physicians’ self-reported Spanish language ability; and the need for national training and certification standards for professional health care interpreters. She has served as an advisor to numerous national foundations, the AMA, ABIM, and other stakeholders focused on health disparities and to state and national advisory committees focused on language barriers and cultural competence. Dr. Fernandez served on the Society of General Internal Medicine Council (2006-09). In addition to her research-related policy work, Dr. Fernandez serves on the board of trustees of American Civil Liberties Union-Northern California.
Liz Goldman, MD
Dr. Goldman’s research and policy work focuses on improving the quality of health care for underserved communities and the safety-net in particular. She promotes high quality, cost-conscious, and appropriate care in the safety-net, and evaluates innovations and health delivery approaches to improve care transitions and provider communication across settings and specialties. As part of her work to improve the science of quality measurement, she has served on an expert work group for Agency for Healthcare Research and Quality Present on Admission (POA) Project.
Claire Horton, MD
Dr. Horton's policy and advocacy work centers on primary care re-design in safety net settings, the elimination of racial and ethnic disparities through primary care quality improvement (QI) efforts, and coaching physician leaders to create system-level change. She launched and co-directs (with Dr. Urmimala Sarkar) the "Triple AIM" curriculum for primary care internal medicine residents at SFGH. The curriculum introduces residents to core QI concepts and skills and includes an experiential component in which residents complete clinic-based QI projects. She is part of UCSF/Center for Health Professions' ACTION grant network, which focuses on integration of health disparities data into QI initiatives. She serves on the advisory board for Healthy San Francisco / San Francisco Health Plan's Quality Improvement initiatives, which have been instrumental in helping to create Pay-for-Performance initiatives in the San Francisco safety net. In the past she has also served on California's Medicaid Managed Care advisory board. She is a coach for the UCSF Center for Health Professions' Institute for Physician Leadership, which aims to equip California's physician leaders with leadership skills to lead their organizations and create meaningful change in statewide healthcare systems (http://www.futurehealth.ucsf.edu/Public/Leadership-Programs/Home.aspx?pid=65)
Leigh Kimberg, MD
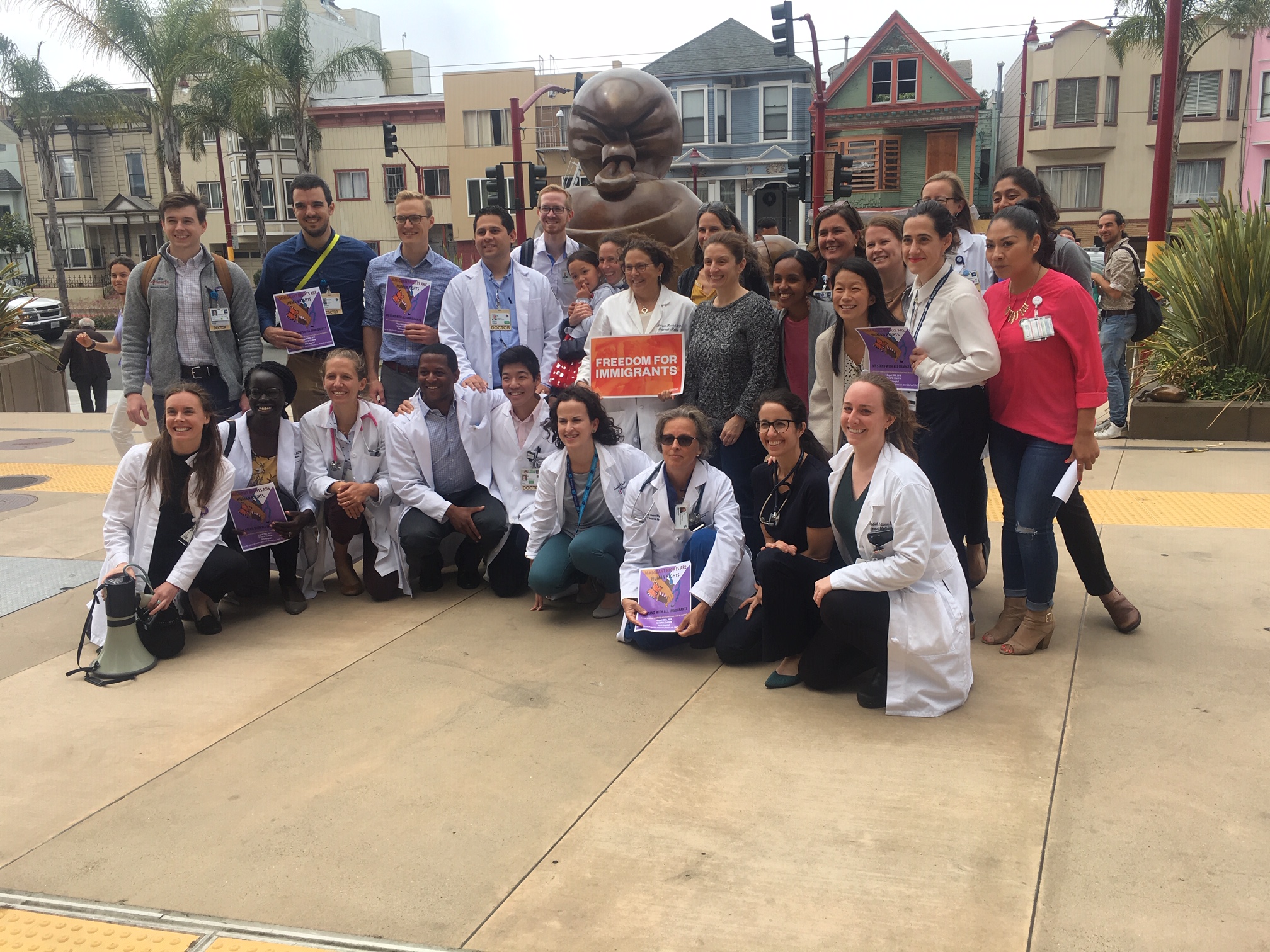
Dr. Leigh Kimberg’s policy and advocacy work focuses on violence prevention, increasing enrollment of medical students from historically excluded communities, and advancing anti-racist, anti-oppression health professions education. She has worked on policy and advocacy initiatives to prevent and mitigate the adverse effects of violence and trauma and promote models of healing-centered, trauma-informed healthcare. Dr. Kimberg has served on national advisory boards convened by Futures without Violence (previously the Family Violence Prevention Fund) to develop national guidelines on addressing intimate partner violence in healthcare practice; she has also advocated for these guidelines to be adopted and implemented locally. She garnered federal funding to study the implementation of the Affordable Care Act’s mandate to provide all girls and women with IPV counseling and services. Dr. Kimberg serves as the San Francisco Department of Public Health (SFDPH) representative to the Board of Supervisors mandated San Francisco Family Violence Council (SF FVC) to advance violence prevention and intervention policies in collaboration with other governmental and community-based organization partners. Recently, Dr. Kimberg has been engaging in abolitionist advocacy to eliminate policing in healthcare, including in SFDPH. As the Program Director for Program in Medical Education for the Urban Underserved (PRIME-US) at UCSF and the UCB-UCSF Joint Medical Program, she participates in policy and advocacy efforts to recruit and equip students from historically excluded communities to become physician health equity leaders. She is also privileged and honored to have the opportunity to actively support the policy and advocacy efforts of the PRIME-US students, who are national leaders in many areas including anti-racist medical education and healthcare, access to care, immigrant’s rights, DACA, and more.
Margot Kushel, MD
Dr. Kushel’s policy work focuses on addressing housing as a key social determinant of health. Her work aims to create the evidence base for policy responses to prevent and end homelessness and mitigate the effects of housing instability on health. Dr. Kushel works with diverse stakeholders at the local, regional, and national level to inform and implement programmatic and policy changes based on her research, which focuses on the causes and consequences of homelessness in older adults and the effects of various housing interventions on health care utilization and health outcomes. She has provided testimony at California state legislative committees, presented her findings at local, regional, and national conferences, and is a frequent speaker to medical and lay audiences on highly vulnerable populations both in person and through traditional and new media. She is a leadership board member of Everyone Home, which coordinates homeless policy in Alameda County. She serves as an evaluator of multiple initiatives seeking to address homelessness, including Santa Clara’s Pay for Success funded supportive housing initiative, Tipping Point’s Chronic Homelessness Initiative and Whole Person Care in San Francisco.
Courtney Lyles, PhD
Dr. Lyles’s policy work currently focuses on health information technology implementation and digital inclusion, specifically patient engagement and digital/health literacy among vulnerable populations. Dr. Lyles advocates for the design and dissemination of better health information technology tools for vulnerable patients, through better skills training and support, increased usability standards, and metrics that demonstrate true patient engagement. Here are a few recent highlights:
Focusing on Digital Health Equity (JAMA Viewpoint)
Tackling digital inequality in the tech capital of the world (SF Examiner)
Nynikka Palmer, PhD
Dr. Palmer’s policy and advocacy efforts are centered around achieving health equity for high-quality care for African American men facing prostate cancer. Her work sits at the intersection of multiple fields and methods, including cancer disparities, health services research, health care communication, and community engagement. She launched an African American prostate cancer support group, as none existed in the Bay Area, with the mission to provide a safe and supportive place where men can come together for dialogue and education. With a roster of over 90 African American men, this group has been thriving since 2014. As co-leader of the SF CAN Prostate Cancer Task Force, the group is leading efforts for Smarter Screening and Smarter Treatment for prostate cancer, to eliminate sub-optimal screening practices and treatment in African American men through community and health care system partnerships.
Neda Ratanawongsa, MD
Dr. Ratanawongsa's advocacy work has focused on system redesign to support safety net clinicians in developing meaningful therapeutic alliances with their patients. Specifically, she is interested in assuring that quality measures, incentives, and health system policies promote relationship-centered communication, support clinician well-being, and improve the recruitment and retention of diverse clinicians in the safety net workforce. Dr. Ratanawongsa's current focus is on tailoring electronic health record system implementation metrics to meet the needs of clinicians caring for linguistically and culturally diverse populations.
Urmimala Sarkar, MD
Dr. Sarkar’s policy and advocacy work focus on the areas of patient safety, specifically for vulnerable populations with chronic conditions, and health information technology. She serves as an advisor to the National Patient Safety Foundation on outpatient issues and recently served on a Technical Expert Panel on ambulatory safety for the U.S. Department of Health and Human Services. In addition, Dr. Sarkar is passionate about harnessing the health information technology revolution to reduce racial/ethnic, economic, and literacy-related disparities in health care by innovating to address the unmet need for appropriate patient-facing technologies for vulnerable populations.
Dean Schillinger, MD
Dr. Schillinger has a long history of successfully advocating for healthcare and public health policies to enhance health communication for health equity in a variety of domains, including patient safety, health literacy, and digital communication. Dr. Schillinger is also a leading scientific and public health expert on the root causes of the global diabetes epidemic and has been instrumental in engaging the scientific community in the critical policy discourse related to the dangers of unmitigated added sugar consumption. Because of his diabetes public health expertise, he served as the scientific expert for the City and County of San Francisco in the successful defense of a lawsuit filed in Federal Court by the American Beverage Association for an injunction against a city ordinance to mandate health warning labels on billboards advertising sugary drinks. As a result of the City’s successful defense, the first sugary drink warning label law in the world will go into effect in 2017 (1) requiring health warnings on advertisements for sodas and other sugary drinks (2) banning such advertising on city property and (3) prohibiting the city from spending money on sugary drinks. Dr. Schillinger has recently authored a number of widely-read original investigations as well as influential public health policy pieces in the Annals of Internal Medicine and JAMA that describe how the sugary beverage industry has been manipulating disparate elements of the scientific process to undermine scientific claims of their products’ health consequences and to create controversy regarding the scientific basis for placing dietary limits on added sugars. To directly engage the affected communities in the emerging crisis of Type 2 diabetes in America’s children, Dr. Schillinger co-created a minority youth-led public health literacy campaign to prevent diabetes that employs social media and spoken word, The Bigger Picture (http://www.thebiggerpicture.org/), which was highlighted at a 2013 IOM Health Literacy Policy Roundtable event, was awarded the Spirit of 1848 Award from the American Public Health Association and recently received the WHO NCD Policy Innovations Award. An innovative marriage of Public Health and the Arts, The Bigger Picture has been evaluated by his team, and results demonstrate its positive impacts on minority youth and youth stakeholders. The Bigger Picture campaign has had >1.5 million views to date, has been adopted by 3 California counties for their initiatives to reduce sugar-sweetened beverage consumption, and was influential in the passage of sugary drink taxation policies in 4 Bay Area municipalities through its engagement of minority voters. In 2016, Dr. Schillinger received the prestigious James Irvine Leadership Award of California for his groundbreaking work in advancing the public health literacy of Californians with respect to the diabetes epidemic. Dr. Schillinger has also served as a consultant to Navajo Nation, the Ministry of Health in Israel regarding their diabetes prevention efforts, and to the Ministry of Health in Singapore after it declared a “War on Diabetes”. His efforts led to Singapore becoming the first nation in the world to ban advertising of sugary drinks. Finally, Dr. Schillinger served as co-chair of the Congressionally-chartered National Clinical Care Commission whose purpose was to prepare and submit a report on how US federal agencies can be better leveraged to prevent and control diabetes. He was in charge of the sub-committee making recommendations on all non-health agencies (e.g. HUD, USDA, Dept of Education, FTC, etc.) on behalf of an all-government approach to diabetes prevention and control.
Hilary Seligman, MD
Dr. Seligman’s policy and advocacy expertise focus on federal nutrition programs (predominantly the Supplemental Nutrition Assistance Program), community food programs (food vouchers, food banks, and food pantries), food affordability and access, and income-related drivers of food choice. She serves as Senior Medical Advisor for Feeding America, the nation’s largest domestic anti-hunger organization. She directs the CDC’s Nutrition and Obesity Policy Research and Evaluation Network (www.nopren.org). She also founded San Francisco’s fruit and vegetable voucher program, EatSF (eatsfvoucher.org), which has since expanded to other cities as Vouchers for Veggies.
Maya Vijayaraghavan, MD
Dr. Vijayaraghavan’s policy work is focused on tobacco control policy, with an emphasis on vulnerable populations. She analyzes national cross-sectional and longitudinal data to examine the differential impact of tobacco control policies on low-income populations in the US. Dr. Vijayaraghavan is interested in the implementation of smoke-free policies in subsidized housing, including permanent supportive housing for persons who were formerly homeless and for other forms of subsidized housing including Housing Choice Vouchers or subsidized housing in the private rental market. She is currently the PI of a grant funded by the National Cancer Institute on conducting a cluster randomized controlled trial of a smoke-free home intervention in permanent supportive housing for formerly homeless in the San Francisco Bay Area. Dr. Vijayaraghavan’s broader tobacco control policy work also encompasses system-level approaches to increase access to cessation services for low-income populations in the US. She is the PI of a grant funded by the Tobacco Related Disease Research Program to conduct a pilot randomized controlled trial of a contingency management intervention for patients experiencing homelessness who are engaged in clinical care at the Tom Waddell Urban Health Clinic in San Francisco, CA. This intervention is integrated within the clinic’s Epic electronic health record. She is also a co-investigator on a grant funded by the Tobacco Related Disease Program on developing system level approaches using the electronic health record to increase delivery of cessation services to patients in safety net health systems. Using these approaches, her team has developed ways to estimate quit attempts at population level among primary care patient populations as well as integrating health systems with population-level interventions such as the state tobacco quitline. Her most recent project is focused on the integration of smoking.